Improved health outcomes and quality of life
Care for Managing Dementia for Elders
Content is medically reviewed by:
Dr. Shakti Singh
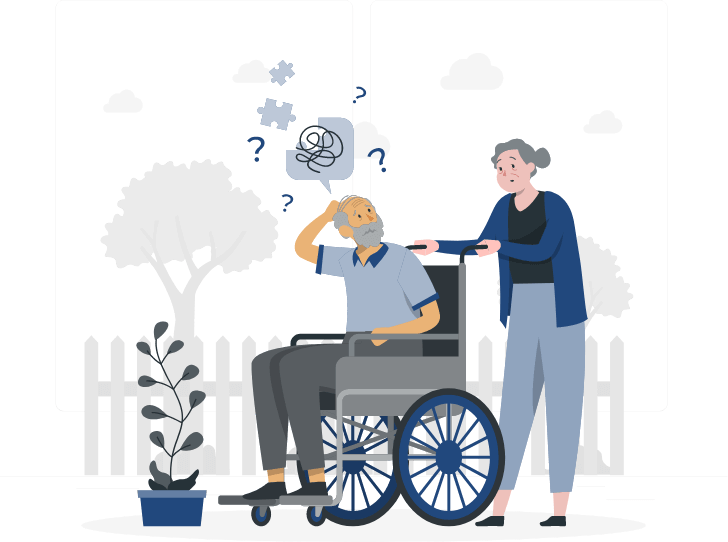
What is dementia?
Becoming somewhat forgetful is a part of the natural aging process. Subtle changes in memory or absent-mindedness due to aging are not the same things as dementia. Dementia impacts much more than memory, and managing dementia calls for a medical evaluation.
Memory losses and cognitive declines that are severe enough to interfere with daily life activities are called dementia. In other words, it is an umbrella term for a persistent and disabling decline in functional and intellectual abilities of memory, language, judgment, and thinking. Dementia becomes increasingly common as people age, and only worsens over time. Dementia care thus emphasizes the importance of holistic care for an elderly’s well-being‒social, mental, and emotional, in addition to physical and medical needs. There are different types of dementia, the most common of which is Alzheimer’s Disease (AD).
Difference Between Dementia and Alzheimer's Disease:
While dementia is a broader term for cognitive health decline, Alzheimer’s is a specific disease and the most common form of dementia. The table below highlights the key differences between the two.

Dementia is a progressive disorder and brings diverse challenges for the patients‒from communication to behavioural and psychological. Care for dementia patients with comorbidities requires extra supportive and person-centred approach to respond effectively to their needs. In the absence of a cure, long-term dementia care is the only alternative to maintaining the quality of life. In addition, recent research also shows that dementia patients with high continuity of care have better health outcomes and lower rates of complications. Qualitative dementia care focuses on:
-
-
Lowering the risk of complications like delirium, drowsiness, and falls
-
Reduce hospitalization and treatment costs
-
Providing peace and stability to the patient and family members
senOcare’s guide to managing dementia and cognitive health: Case studies and tips

A loved one with dementia in the family can cause stress and uncertainty for everyone involved. Dementia care is complex, and caregivers must understand the different types of dementia, its stage, and the rate of progression. The following are some real-life cases that highlight the importance of person-centered care in the spectrum of dementia and other cognitive impairment across age-groups. It should be noted that all names of patients in the cases have been changed to protect the patients’ confidentiality.
Case Study 01
Gayatri Devi is a 77-year-old female dementia patient with a history of forgetfulness, repetitiveness, and delusions. She would often call her husband every five minutes and forget about the event of calling him. She does not remember dates but remembers events of her life.
She suffered from delusions that would make her suspicious about house helps, especially about theft or being negligent of their duties. It makes her apprehensive about hiring any outside help. This delusion disorder would also make her get lost in her neighbourhood and hence cannot step outside alone.
After a holistic assessment of the situation, our assistance for the best dementia care for Ms. Devi included a host of measures:
- Being compassionate and patient while taking care of her day-to-day needs
- Refrain from anger or agitation even if she asked repetitive questions numerous times a day. Speaking slowly in a soft tone and act as if it’s the first time
- Educating other family members about her behaviour which is not under the elder’s control, including examples of what to say and what not to say in various situations
- Started treating her with the same care and compassion as one would treat a child
Case Study 02
Pawan Behl is a 66-year-old male patient with Alzheimer’s, being referred to our home care for Alzheimer’s patients. Mr. Behl has a medical history of increased memory loss, confusion, and hallucinations. He does not remember his daughter and even forgets to perform his daily hygiene activities of bathing and changing clothes. The extent of his hallucinations would take him back to his early twenties and make him constantly talk to his parents, who are not alive anymore.
He would also set up a dinner table every night for guests. The medical reports state that he has difficulty handling finances or paying bills. His confusion often leads to anger outbursts and aggressive impulses like scratching people around him.
While caring for Alzheimer’s patients, one will encounter feelings of anger, confusion, hallucinations, and even paranoia. These are common in the early stages of Alzheimer’s, and our assessment suggested the following in this case:
- Do all the tasks in breaks so that the patient does not feel exhausted and allow him to do a few things on his own
- Engage and involve the patient in fun and simple activities like choosing from two options.
- Be clear in instructions so that it becomes easy for him to understand
Case Study 03

Nidhi Massey is a 46-year-old female patient with Parkinson’s disease‒‒a progressive neurological disorder that causes movement disorder. Her hands often shake whether they are working or at rest. Due to this, her movement has become slow, and she takes small steps while walking. She also has pain in her muscles. Sometimes she speaks very softly and sometimes very fast.
Recent research has found that 70 percent of people with Parkinson’s will develop symptoms of dementia as a part of the disease progression. To manage symptom control, a caregiver must be vigilant in administering medications with reminders, charts, and organizers. As such, our suggestions were:
- Having conversations with her to understand her needs
- Having conversations with her to understand her needs
- Observing closely and notice changes in her, keeping a check on whether she is taking medicines on time
- Being patient with her
Case Study 04

Ambika Pal Singh, a 75-year-old female, is diagnosed with Post-Traumatic Stress Disorder (PTSD), a behavioural disorder triggered by traumatic events causing fear, helplessness, or horror. As a result, she gets scared of sleeping. Whenever she tries to sleep, nightmares of the past tragic events disturb her taking her back to those events. She always remains emotionally disturbed and leads a reclusive life.
Since recovery from PTSD is gradual, patience and support from others are the key factors. Based on our assessment and expertise, we suggested the following:
- Try to engage her in a conversation as much as possible and be a good listener
- Supporting and encouraging her on every point
- Stay connected and be patient
Managing Dementia: General Care giver tips
We at senOcare understand that the process of aging is not unique, and no two elderly are the same. There is no silver bullet answer to managing dementia because any elderly at any given stage could be suffering from more than one health issue. Hence, each elderly with dementia or cognitive impairment represents a unique condition, and so is the situation in which they find themselves. It’s not something in their control, it’s the condition, and thus patience is the key. You must allow some time to let them have their way. Some general tips that can come in handy are:
-
Establishing a routine of hygiene activities
-
Maintain a safe and uncluttered environment
-
Use simple words and sentences
-
Act with affection, reassurance, and patience
-
Avoid agitation or resentment from your end
What our Happy Customers Say
Media Coverage







Looking for a trusted team who can take care of your parents' day to day needs?
Speak to our Care Manager now!
FAQs
-
Q1. Can a Dementia Person be cared for at home?
YES. In-home care for dementia patients provides one-on-one routine care and supervision. Familiar surroundings also offer greater security and peace of mind to people with memory and cognitive issues. Research also shows that in-home care is worth considering in the early stages of Alzheimer’s disease (AD) or other forms of dementia to help the patients stay healthier and happier.
-
Q2. When should dementia patients go into care?
Dementia is a progressive disease, meaning that it would only worsen over time. When a patient becomes aggressive, or the condition deteriorates to the point where they need a high level of medical care, it could be time to consider nursing home dementia care.
-
Q3. Do dementia patients do better at home?
YES. If care is provided at an early stage, dementia care at home helps the patient live longer and happier. Home care is considered ideal because of:
- Familiarity with and comfort in their surroundings
- One-on-one care and attention leading to better outcomes
- Security and peace of mind to patients and their families
- Safe environment in the wake of Covid-19
- Cost-saving when compared with assisted living or nursing home facilities
-
Q4. What is the range of Senocare’s Dementia care service?
Our compassionate Care Managers are trained to deal with any circumstances, however unpleasant it may be. The range of dementia care includes medical and non-medical care like:
- Medication management
- Safety concerns and counselling
- Nursing care for dementia patients with comorbidities
- Monitoring for depression, anxiety, or stress
- Nutrition and physiotherapy support
- Helping with daily hygiene activities
- Companionship
-
Q5. How long can a Dementia person live at home?
Experts recommend that dementia care at home can continue through to the end of life. However, the situation varies, and disease progression is unique in each case. Hence, home care may not always be possible for patients who need full-time medical support or constantly putting their physical safety at risk.
-
Q6. What is the best care for dementia patients?
Dementia care is complex, and the best care depends on the stage and progression of the disease. What may work today may not work tomorrow. In addition, an elder at any stage could be suffering from more than one health issue, making it more challenging. Some general tips that can come in handy are:
- Establishing a routine of hygiene activities
- Use simple words and sentences
- Maintain a safe and uncluttered environment
- Respond with affection, reassurance, and patience
-
Q7. When do dementia persons need assisted care?
Dementia care is a full-time responsibility, and a caregiver needs to be mindful of various factors like personal care, safety concerns, mood swings, etc. over and above medication management. All these can be stressful to manage on your own. Since it is a progressive disease, care requirements can become more intensive and complex in the advanced stages. While it may never feel like the “right time” for assisted care, if introduced earlier, dementia care at home can help the patient to live longer and happier.
-
Q8. What is the procedure to request for Dementia care?
Our elder care home services plans‒Senocare Touch Of Love, Senocare COMFORT, and Senocare INDULGE have been designed to meet the wide spectrum of elderly care. From dementia care to Parkinson’s, or care for any other psychological ailment, you can choose the one that fits your requirements. For further information on our customized packages, please reach out to us at [email protected].
-
Q9. How is Dementia Caused?
Dementia is caused by damage to brain cells, impacting their ability to communicate effectively. The most common cause is Alzheimer’s disease, but other factors such as vascular dementia, Lewy body dementia, and frontotemporal disorders can also contribute.
-
Q10. What are the 5 Signs of Dementia?
The five common signs of dementia include memory loss, difficulty in communication and language, challenges in focusing and reasoning, visual perception issues, and impaired judgment. Recognizing these signs early is crucial for effective management.
-
Q11. Is Dementia Caused by Age?
While age is a significant risk factor, dementia is not solely caused by aging. It is more prevalent in older individuals, but factors like genetics, lifestyle, and overall health play a role. Younger individuals can also experience early-onset dementia.
-
Q12. Is Dementia Curable?
As of now, there is no cure for most types of dementia. However, early diagnosis and appropriate management can significantly improve the quality of life for individuals living with dementia.
-
Q13. How to Avoid Dementia?
Although dementia risk cannot be entirely eliminated, certain lifestyle choices can reduce it. Maintaining a healthy diet, engaging in regular physical exercise, staying mentally active, managing cardiovascular health, and fostering social connections are ways to support brain health.
-
Q14. Is Dementia Genetic?
Genetics can play a role in some types of dementia. Individuals with a family history of dementia may be at a higher risk, but lifestyle factors still contribute significantly to the overall risk.
-
Q15. What are the 1st Signs of Dementia?
The initial signs often include subtle memory loss, difficulty in finding the right words, challenges in planning and problem-solving, and a decline in the ability to complete familiar tasks. Recognizing these signs early allows for timely intervention.
-
Q16. Can Stress Cause Dementia?
While stress itself may not directly cause dementia, it can contribute to cognitive decline and impact overall brain health. Chronic stress can exacerbate existing conditions and increase the risk of developing dementia.
-
Q17. Do People with Dementia Sleep a Lot?
Sleep disturbances are common in dementia, but the relationship between dementia and sleep is complex. Some individuals may experience increased daytime sleepiness, while others may face nighttime sleep disturbances.
-
Q18. What are the 3 Best Foods for Memory Loss?
Foods rich in antioxidants, omega-3 fatty acids, and vitamins E and C are beneficial for brain health. Examples include berries, fatty fish (like salmon), and nuts. A balanced diet that supports overall health is crucial.
-
Q19. What are the 7 Habits to Avoid Dementia?
Maintaining a healthy lifestyle involves habits such as regular exercise, a balanced diet, staying mentally active (e.g., puzzles or learning new skills), managing stress, getting quality sleep, staying socially connected, and avoiding excessive alcohol consumption.

